HIPAA-Critical Contract Mistakes Healthcare Must Avoid
Even the most well-structured agreements can unravel if the basics aren’t handled carefully.

Data privacy failures in healthcare are rarely small. They trigger lawsuits, regulatory penalties, and reputational damage that takes years to recover from.
The case of Flo, once Europe’s leading femtech app with 380M+ users, is a clear warning. A data privacy lapse around PHI (protected health information) led to a class-action lawsuit and a permanent dent in brand trust.
Healthcare organizations like hospitals, healthtech startups, and even insurers face similar risks every day. The stakes are too high for healthcare contracts to feature any lapses.
This blog explores where mistakes commonly occur, why they escalate into costly problems, and how you can reduce compliance risks with the right contract management.
Common Mistakes that Put Healthcare Contracts at Risk

Even the most well-structured agreements can unravel if the basics aren’t handled carefully.
In healthcare, where every contract touches sensitive data, compliance standards, or patient outcomes, even minor mistakes can quickly escalate into lawsuits, penalties, or operational disruptions.
The risks often hide in everyday processes, like how contracts are stored, updated, or shared, and become visible only when regulators or auditors come knocking.
These are the core pressure points you need to watch:
Privacy and Data Protection Lapses
Every agreement touches PHI. Without clear terms for encryption, access control, and data sharing, you expose your organization to HIPAA violations and GDPR penalties. Even minor oversights can snowball into million-dollar settlements.
Missing Regulatory Updates
Whether it’s HIPAA, GDPR, telehealth billing, or cross-border storage rules, the compliance landscape changes constantly. When contracts aren’t regularly updated, organizations often find themselves technically non-compliant long before an audit makes it visible.
Multi-Party Blind Spots
Healthcare is an ecosystem encompassing hospitals, insurers, labs, and IT vendors. Each works separately. Without a single official reference for each party’s obligations, renewals, or compliance clauses, it’s nearly impossible to confirm that everyone is aligned.
Audit Readiness Failures
Regulators and accreditation bodies often demand clause-level history: who changed what, when, and under whose authority. Email chains and disconnected files can’t provide this. The result is a signal of weak internal control.
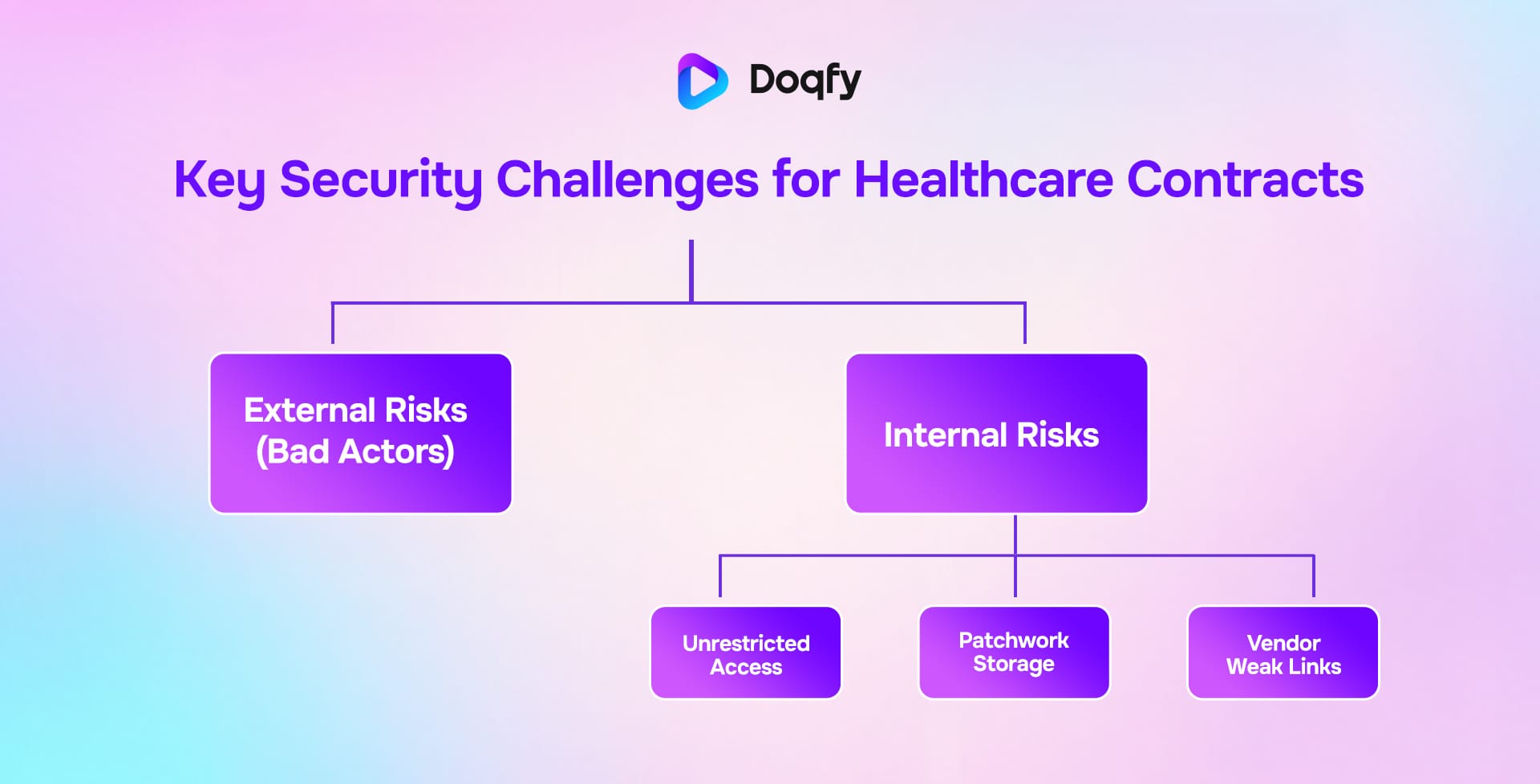
The Security Challenges You Must Not Ignore
Healthcare contracts are a prime target for cyber attacks, as they often contain patient identifiers, insurance details, payment obligations, and vendor access credentials.
Yet, too many contracts sit in unsecured drives or folders without encryption.
External risks
Hackers target PHI because it’s more valuable than financial data. An unsecured contract repository becomes an easy entry point. However, external threats are only half the story. The real risk often lies inside the organization.
Internal risks
Employees with excessive access privileges can accidentally (or intentionally) expose sensitive data. Without role-based controls, there’s no way to prevent it. Internal risks can be broadly classified into 3 major threats, viz:
Unrestricted access
Contracts stored on shared drives without role-based permissions expose data to employees who don’t need to see it.
Patchwork storage
Jumbled storage across emails, thumb drives, and traditional systems makes it impossible to enforce consistent security standards across hundreds or thousands of agreements.
Vendor weak links
Third-party service providers often access healthcare data through contracts. If those agreements don’t enforce modern security protocols, they become open doors for breaches.
A breach here is never “just legal’s problem.” It interferes with end-user care delivery, hurts patient trust, and creates cascading operational failures that affect every stakeholder.
How You Can Manage Healthcare Contracts Smarter
Instead of adding more oversight meetings or expanding compliance teams, the real fix is a system that reduces errors and enforces standards across every contract.
Here’s a quick guide on how you can implement that:
Centralize storage
Secure repositories with encryption and role-based access keep contracts controlled yet accessible.
Automate compliance tracking
Built-in alerts ensure renewals, clause reviews, and new regulations don’t fall through the cracks.
Standardize clauses
Templates aligned with HIPAA and regional laws reduce human error and maintain consistency.
Maintain audit trails
Every signature, edit, and access point is logged automatically for instant audit readiness.
By embedding compliance into the process, CLM transforms contracts from hidden liabilities into an operational safety net.
Conclusion
Healthcare contracts sit at the intersection of compliance, patient trust, and operational continuity. A single lapse in privacy clauses can trigger HIPAA, GDPR or CEA violations.
A missed update to regulations can leave providers out of compliance overnight. Disconnected systems create blind spots across multi-party agreements, and weak storage practices open the door to costly breaches.
Audit and compliance readiness is really about proving control, consistency, and accountability in every agreement. Without that foundation, your healthcare organization faces both financial penalties and the erosion of public trust.
The solution lies in making your contracts act as more than documentation of agreements. The key lies in turning them into strategic, managed assets that protect sensitive data, align with evolving regulations, and remain secure under scrutiny.
Protecting patient trust starts with protecting contracts. Explore how Doqfy helps healthcare organizations achieve compliance without compromise. Book a demo today!
References
- Flo Health settles multi-billion dollar Meta data privacy lawsuit | Sifted
- Flo Health makes Flo Premium available for free for 1 billion women worldwide
- Flo Health settles class action over personal health data sharing | ICLG
- Jury Rules Meta Violated California Privacy Law by Collecting Flo App Users’ Sensitive Data

